Specimen collection and quality are undoubtedly among the most critical steps in diagnosing a disease. This is because the method of sample collection and quality of samples obtained significantly affects the results of the diagnostic tests and, hence, the accuracy of diagnosis. In turn, this influences the appropriateness and effectiveness of medical care delivered to patients.
A study performed in 2018 reported that the overall laboratory error rate is 0.3%; 65% of which were due to pre-analytical errors, which includes1:
- Inappropriate sample volume
- Poor sample collection
- Poor sample handling and processing
- Poor sample quality
Different types of samples — blood, urine, skin swabs, swabs from mucosal surfaces (e.g., nose, throat), feces, sputum, synovial fluid — utilize different collection methods. These sampling methods require different techniques to minimize acquiring a poor-quality specimen sample. What exactly is a poor-quality specimen? Generally, a poor-quality specimen could refer to:
- Specimens in which causative microorganism (s) have failed to be detected — This is usually caused by poor sampling techniques (e.g., samples of the edges of the ulcer instead of the center, blood samples obtained after starting antibiotic treatment, superficial swab instead of deep biopsy or tissue samples).
- Contaminated specimens — Ultimately, contaminated samples could result in false-positive diagnostic results.
Sample Contamination
A contaminant is defined as microbes introduced to the samples during sample collection or processing that are not pathogenic for the patient and, therefore, are not involved in disease pathogenesis. Poor quality specimens remain a significant obstacle for traditional cultures and PCR and sequencing-based diagnostics.
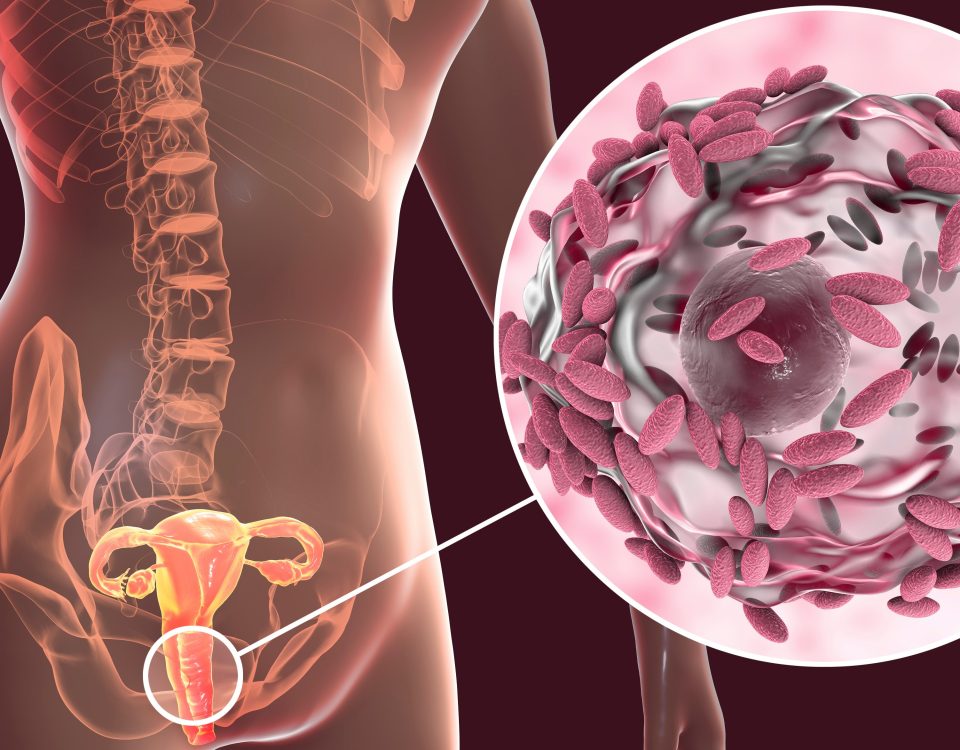
The source of sample contamination could be from adjacent areas of the body (e.g., skin when taking a wound sample, the vagina when taking a urine sample) or external sources such as the packaging of collection materials. The human skin is home to a wide variety of microflora, mainly composed of non-pathogenic microbes. However, the microflora can enter and contaminate specimens because of poor sample collection techniques.
A study published in the Journal of Emergency Nursing reported that 30% of urine cultures obtained were contaminated.2 The median urine sample contamination rate in the United States is about 15%.3 Another recent study reported that 10% of their Tuberculosis sputum samples were contaminated with non-tuberculosis bacteria and fungi, which dominated the samples.4.
The presence of certain health conditions could also influence the risk of sample contamination. For example, it was found that midstream urine specimens obtained from women with pelvic organ prolapse were more likely to be contaminated.5
Sensitivity of NGS-Based Diagnostics
Next-generation sequencing (NGS) is an advanced molecular diagnostic tool capable of sequencing the entire genome within days,6 allowing for comprehensive detection and identification of microorganisms in patient samples. MicroGenDX, the leader in molecular diagnostics of infections, offers qPCR+NGS diagnostic solutions to diagnose a plethora of infections accurately.
Typically, samples are lysed to extract microbial DNA. DNA is then purified to ensure that it is free from contaminating RNA, proteins, and nucleases. The DNA samples are then used for qPCR and preparation of the sequencing library, which is used for sequencing every DNA fragment present in the sample.
Therefore, MicroGenDX’s qPCR+NGS diagnostic tool can pick up microbes that are present even in minute amounts. This is significant as conventional culture conditions may not be able to support the growth of and select for certain types of microorganisms, therefore decreasing the accuracy of the diagnostic test.
The high level of sensitivity of NGS has allowed for better detection of infection-causing pathogens, such as in the case of acute cystitis.7 However, because NGS is a highly sensitive and accurate tool, contaminating microbes such as skin microflora will be readily detected. As a result, sample collection and quality are exceptionally critical to reducing rates of false positives in NGS-based diagnostics.
General Precautions When Collecting Specimens for NGS Diagnostics
As mentioned above, different types of samples require different methods and precautions to ensure specimen quality. Nonetheless, there are general guidelines that can be followed to help increase the quality of specimens that are collected for NGS diagnostics:
- Wherever possible, collect specimens before administering antimicrobials: The administration of antimicrobials will alter the composition of microorganisms, making data analysis and interpretation difficult. It is possible to collect viable NGS specimens after antimicrobials are administered but depending on sample type not optimal. Only the proscribing healthcare provider should make the decision to delay or interrupt treatment.
- When appropriate, decontaminate the skin surface with disinfectants such as 70% alcohol: This will markedly reduce the likelihood of contamination by skin microflora.
- Collect specimens from the actual site of infection (e.g., the center of the infected area instead of the edges, appropriate sampling techniques for infections such as joint infections8): Increases the likelihood of sampling the pathogenic microbes in the infected area.
- The samples should not come into contact with the containers or any packaging materials: Prevent contamination from external sources.
There are also other sample-specific guidelines9 that could aid in minimizing the risk of sample contamination.
Importance of Quality Control and Curated Database
MicroGenDX provides additional resources to facilitate the collection of different samples using the kits that are provided with the diagnostic services. Written and video instructions are available for the collection of a wide range of specimens, including COVID-19, blood, ENT, GI, nail, orthopedics, pulmonary, urology, women’s health, and wound care samples.
Quality control is also included in MicroGenDX’s NGS workflow — positive and negative controls are used to ensure the quality of the sequencing reads. Additionally, MicroGenDX has an in-house curated database of over 50 thousand species of bacteria and fungi. This database allows for the identification of potential contaminants that are in the patient samples. Also, MicroGenDX provides consultation services directly to physicians, that will aid in better understanding the qPCR+NGS report in terms of abundance and distribution of microbes, dominant species, Etc., and evaluating the clinical significance of report results.
Conclusion
Specimen collection and quality significantly impact diagnostic results. Especially when sensitive molecular diagnostic tools such as NGS are utilized, an abundance of care has to be given to ensure samples are collected appropriately to deliver accurate diagnoses to patients. Physicians should work with their patients to ensure that they are cognizant of specimen contamination risks and consequences, especially when the specimens are self-collected.
MicroGenDX’s qPCR+NGS diagnostic solution has a stringent QC process built into the sample processing workflow and utilizes a curated database to identify and evaluate the abundance of contaminating and non-contaminating microbes.
Literature Sources
- Najat D. Prevalence of Pre-Analytical Errors in Clinical Chemistry Diagnostic Labs in Sulaimani City of Iraqi Kurdistan. PLoS One. 2017;12(1):e0170211. doi: 10.1371/journal.pone.0170211.
- Lough ME, Shradar E, Hsieh C, Hedlin H. Contamination in Adult Midstream Clean-Catch Urine Cultures in the Emergency Department: A Randomized Controlled Trial. Journal of Emergency Nursing. 2019;45(5):488–501. doi: 10.1016/j.jen.2019.06.001
- Bekeris LG, Jones BA, Walsh MK, Wagar EA. Urine culture contamination: a College of American Pathologists Q-Probes study of 127 laboratories. Arch Pathol Lab Med. 2008;132(6):913–7. doi: 5858/2008-132-913-UCCACO
- Muzanyi G, peace A, Wamuntu B, Joseph A, Nassali J. The threat of persistent bacteria and fungi contamination in tuberculosis sputum cultures. Afr Health Sci. 2021;21(2):628–32. doi: 4314/ahs.v21i2.18
- Soriano A, Sansone S, Arora E, Arya L, Andy U. Risk of Contamination of Voided Urine Specimen in Women With Pelvic Organ Prolapse. Female Pelvic Med Reconstr Surg. 2020;26(8):488–92. doi: 1097/SPV.0000000000000760
- The MicroGenDX NGS Process – Perfected by Experience and Continuous Quality Improvement.
- McDonald M, Kameh D, Johnson ME, Johansen TEB, Albala D, Mouraviev V. A Head-to-Head Comparative Phase II Study of Standard Urine Culture and Sensitivity Versus DNA Next-generation Sequencing Testing for Urinary Tract Infections. Rev Urol. 2017;19(4):213–20. doi: 3909/riu0780
- Sousa R, Carvalho A, Santos AC, Abreu MA. Optimal microbiological sampling for the diagnosis of osteoarticular infection. EFORT Open Rev. 2021;6(6):390–8. doi: 1302/2058-5241.6.210011
- Community Infection Prevention and Control Policy for Care Home Settings: Specimen collection.