Patient Billing Information
After providing test results to your physician, MicroGenDX will bill most insurance companies for the testing. The insurance company will review the claim and determine your responsibility for deductible amounts and uncovered portions of the bill for each sample sent to the laboratory. Most MicroGenDX tests are covered by Medicare, select Medicaid, and private insurance.
Please be advised that, if contracted with MicroGenDX, your insurance will provide us the amount to bill you for the services rendered. This amount could vary depending on your plan deductible, coinsurance and/or copay, and may be higher than our discount offered to uninsured (self-pay) patients. If you have questions or concerns regarding your coverage, please contact your insurance company in advance. We offer a discounted cash price for those patients whose insurance is not contracted with MicroGenDX.
MicroGenDX is committed to ensuring that all physicians and patients have a complete understanding of our billing policies and receive all necessary information to make an informed decision. Our Billing Department is available for any questions or concerns regarding your MicroGenDX bill at at 1-855-208-0019 option #2. The Billing Department is open 8AM to 5PM CST Monday through Friday.
Billing Process for MicroGenDX Services
- After taking the test the patient should sign the patient section of the lab requisition and assist the doctor in providing all necessary insurance information. Please call the phone number on the back of your insurance card for information on coverage of any MicroGenDX test.
- Upon Receiving the patient sample, MicroGenDX verifies insurance information, completes testing, and will issue a courtesy to bill your insurance plan. It is helpful at this stage for the patient to submit their medical records for the test to their insurance plan. Medical records can be obtained by the patient from their doctor.
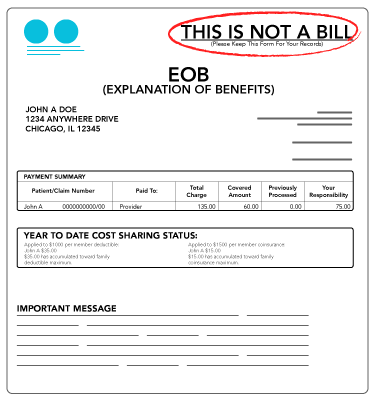
- Insurance providers will then mail patients an Explanation of Benefits (EOB). Please Note an EOB is NOT a bill from MicroGenDX. For some insurances this may not happen in a timely manner. Especially if the patient has not submitted medical records.
- If the insurance plan does not cover the test, or moved forward with the insurance billing process, the patient will receive a bill after 30 calendar days.
- MicroGenDX offers a Patient Assistance Program which allows patients to pay in monthly installments until their balance is paid in full. Contact the Billing Department at 1-855-208-0019 option #2 with additional questions or to begin a payment plan.
If Insurance Provider Sends A Check to You Instead of MicroGenDX
PLEASE NOTE: Several BCBS and GHI Plans may send the check to the patient. Please write “Pay to the Order of MicroGenDX” and send that check directly to our offices at 2002 W. Loop 289, Suite 116, Lubbock TX 79407.
Billing FAQs
General Questions
Please refer to the message on your MicroGenDX invoice or the Explanation of Benefits (EOB) from your insurance carrier for more specific information about why you received an invoice.
A few reasons you may have received an invoice include, but are not limited to, the following:
- Insurance information was not received or the wrong insurance information was received on your test order
- The insurance carrier processed the claim and denied payment
- The insurance carrier processed the claim and applied the balance to your co-pay or deductible
- The insurance carrier did not respond to the claim
Insurance
- Insurance information was not received or the wrong insurance information was received on your test order;
- The insurance carrier processed the claim and denied payment;
- The insurance carrier processed the claim and applied the balance to your co-pay or deductible;
- The insurance carrier did not respond to the claim.
Coverage
Pricing
- If you have insurance or not;
- Your insurance plan coverage of laboratory tests;
- Your age: if you are 65+, Medicare will not always pay for some tests that your physician considers important; and
- Your healthcare providers agreement with MicroGenDX.