Recalcitrant onychomycosis is a fungal nail infection that is prone to relapse. Traditional treatment using potassium hydroxide and culture diagnosis is costly and time-consuming. However, qualitative polymerase chain reaction (qPCR) and next-generation sequencing (NGS) molecular identification methods are extremely specific, quantitative and sensitive, offering superior detection of fungal diversity in fingernail or toenail infections. These methods allow for faster turnaround (up to 3 days) and offer more accuracy in customized treatment of a patient’s cutaneous infection, which can result in better diagnosis and treatment.
Currently, generalized treatment for recalcitrant onychomycosis targets Trichophyton rubrum (T. Rubrum); however, these treatments overlook the other pathogens present in the infection and encourage treatments for the wrong cause; thereby leading to increased instances of drug resistance and prolonged discomfort for the patient.
Recalcitrant Onychomycosis and qPCR + NGS
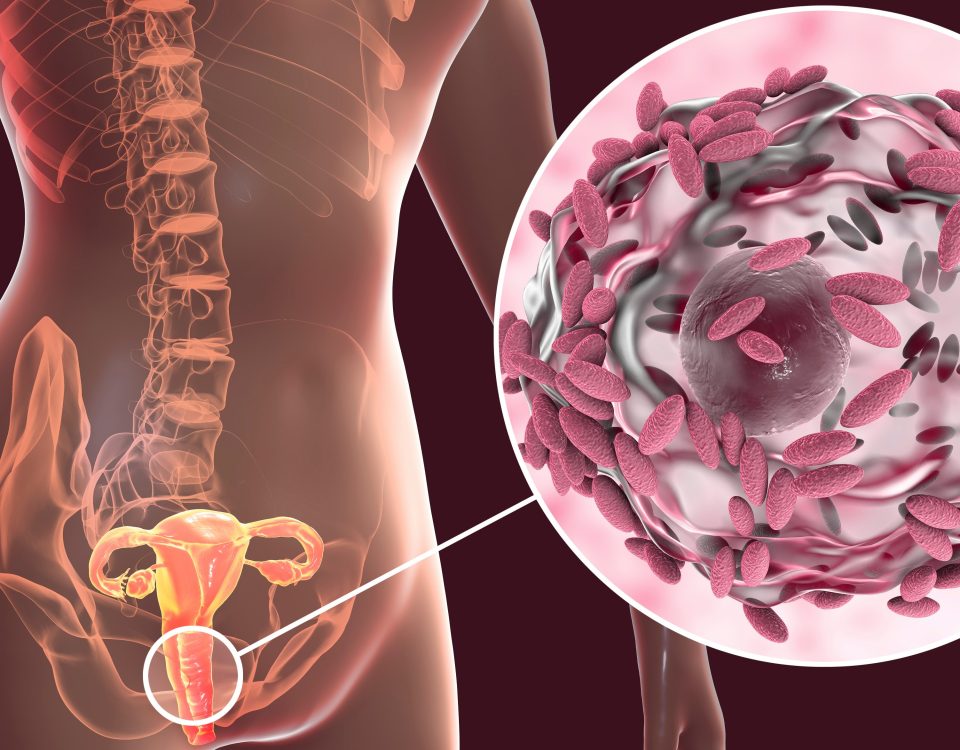
As drug resistance is a growing problem clinically, one way to avoid the increasing evolution of fungi and bacteria is targeted and customized treatment. Before that, an accurate diagnosis of the cause of cutaneous nail infections is imperative. Metagenomics techniques like qPCR and NGS can now determine the entire genetic composition of a microbial community. Dormant or even lowly abundant species can be identified through 16S (bacterial) and 18S (fungal) ribosomal DNA sequences.1
For comparison, in a study of 168 chronic wounds, the culture-diagnostic method identified 17 different bacterial taxa, while molecular testing identified 338 other bacterial taxa.2 Culture is being phased out as an experimental diagnostic method. According to one study of 179 cutaneous infection patients at New York University, culture and histology’s sensitivity were <50%, and only 10% of patients had positive concordance between culture-diagnoses and histology.3 This massive oversight could be indicative of failed treatments and increased drug resistance.
However, with qPCR + NGS tools available to physicians, knowledge of the particular microbe combinations that result in recalcitrant onychomycosis can then be applied to create targeted treatments and improve cure rates. For this reason, molecular genetics-based diagnostics can be used to accurately and rapidly identify microbes present in patients with onychomycosis to improve treatment recommendations.
Molecular Sequencing vs. Cutaneous Toenail Infection Study
In an analysis of a total of 8,816 clinically suspicious toenail samples collected by podiatric physicians from across the United States, next-generation sequencing (NGS) and quantitative polymerase chain reaction (qPCR) were used to identify and quantify dermatophytes, non-dermatophyte molds, and bacteria.1 In this study, approximately 50% of suspicious toenails contained both fungi and bacteria, with the dermatophyte T. rubrum contributing the highest relative abundance and presence in 40% of these samples. This finding was contradictory to the currently accepted and expected estimate of 90%4 in onychomycosis.
Outside of T. rubrum, saprophytic yeasts, NDMs, and bacteria were also observed consistently. Of the remaining 50% of samples, 34% had bacterial species present, and 16% had neither. Other fungi only were present in less than 1 percent of samples. Non-dermatophyte molds contributed to 11% of occurrences in fungus positive samples. All of the control samples were negative for fungi, with commensal bacterial species composing most of the flora population. Because the latter organisms are known to form commensal relationships, there is evidence in the literature to support the theory of a possible group contribution to the disease.1
This case study highlighted the importance of rapid and accurate species-level pathogen detection, using molecular testing techniques such as NGS, in identifying infectious organisms and advising appropriate antimicrobial treatment strategies. To improve treatment outcomes, new molecular diagnostic methods are recommended to confirm the disease and target therapy to the presence of specific microbes.
The Industry Standard vs. the qPCR+ NGS Solution
In recent years, the use of empirical oral terbinafine has been suggested to diagnose the causes of cutaneous nail infection because of the high cost and low accuracy of the prevalent potassium hydroxide and culture technique. However, there are at least two drawbacks to this approach. Firstly, oral and topical antifungal therapies focus specifically on T. rubrum.
As a result, physicians might be contributing to the increased propagation of alternative organisms and encouraging the development of drug resistance by targeting the wrong genus and species. Secondly, other vast but similar nail disorders such as lichen planus, psoriasis, trauma, or others cannot be excluded without nail sampling.1
Alternatively, molecular methods such as MicroGenDX’s qPCR+NGS diagnostic tests are extremely specific, sensitive, and quantitative, which allows for the most accurate diagnosis and invaluable assessments of response to treatment. In the case of nail infections, while qPCR+NGS doesn’t test for disorders like lichen planus and psoriasis, it can rule out infectious causes of dystrophic nails. For example, a “negative” NGS/qPCR result can guide providers away from infectious causes and to look for other causes such as lichen planus and psoriasis with other nail sampling methods (i.e. nail plate/matrix biopsy).
A Physician’s Path to the Best Onychomycosis Diagnosis: MicroGenDX
For quick, accurate, affordable lab results, MicroGenDX is an industry leader in accurate molecular diagnosis of infectious diseases, providing high-quality and reliable quantitative qPCR +NGS-based clinical diagnostic services.
For your next challenging infection, choose MicroGenDX DNA diagnostics. You can expect:
- qPCR in 24-48 hours.
- Targeted identification of a select panel of fungi, bacteria, viruses, and parasites, plus 17 antimicrobial resistance genes
- NGS in 3.5 days.
- Identifies 120 mycobacterial species and over 50,000 bacterial and fungal species
- The most comprehensive diagnostic technology for identifying causal pathogens has never been easier or more affordable
- Reimbursed by Medicare Part B / select Medicaid plans and select commercial insurers
- Discounted patient self-pay
These benefits reduce costs, prevent unnecessary or inappropriate antibiotic usage, and improve patient outcomes.
Resources:
- Annette Joyce DPM, Aditya K. Gupta MD, PhD, FRCP(C), Lars Koenig PhD, Randall Wolcott MD, and Jessie Carviel PhD. Fungal Diversity and Onychomycosis: An Analysis of 8,816 Toenail Samples Using Quantitative PCR and Next-Generation Sequencing. J AM Podiatr Med Assoc. 2019. doi:10.7547/17-070
- Rhoads DD, Wolcott RD, Sun Y, Dowd SE. Comparison of culture and molecular identification of bacteria in chronic wounds. Int J Mol Sci. 2012;13(3):2535-2550. doi:10.3390/ijms13032535
- Shaigany S, Steuer A, Seminara N, Brinster N, Femia A. Comparison between organismal staining on histology and tissue culture in the diagnosis of cutaneous infection: A retrospective study. J Am Acad Dermatol. 2020;82(6):1400-1408. doi:10.1016/j.jaad.2020
- Ghannoum MA, Hajjeh RA, Scher R, ET AL: A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol 43: 641, 2000.
- Feng X, Ling B, Yang X, et al. Molecular Identification of Candida Species Isolated from Onychomycosis in Shanghai, China. Mycopathol 180: 365, 2015.