Urinary tract infections (UTIs) are a common ailment affecting millions of individuals every year. While antibiotics have long been a cornerstone of UTI treatment, the rise of antibiotic resistance is a concerning issue in modern healthcare. Empiric antibiotic therapy, which is prescribed in absence of knowing what pathogens are present, is a standard approach to UTI treatment. However, the effectiveness of empiric antibiotics is dwindling due to rising antibiotic resistance. In this blog, we'll delve into the growing concern of antibiotic resistance, focusing on cephalosporins, potentiated sulfonamides and fluoroquinolones, three of the most commonly used antibiotic classes, and share insights from a recent study by MicroGenDX, which highlights the prevalence of resistance to these drugs.
The Rising Threat of Antibiotic Resistance
Antibiotic resistance occurs when bacteria evolve and develop mechanisms to withstand the effects of antibiotics. This phenomenon is driven by various factors, including overuse and misuse of antibiotics, incomplete treatment courses, and the emergence of resistant bacterial strains. As a result, the antibiotics that were once highly effective in treating UTIs are becoming less reliable.
Cefazolin, Ciprofloxacin, and Sulfamethoxazole-Trimethoprim: Once Effective, Now Challenged
These antibiotics have been staples in the arsenal of antibiotics used to treat UTIs and other infections concerning the genitourinary tract. These drugs have been favored for their broad-spectrum coverage and generally low side-effect profiles. However, data from an internal MicroGenDX study, reveals alarming rates of resistance to these antibiotics in urine samples.
MicroGenDX analyzed over 70,000 urine samples and found the following resistance rates:
- Any Antibiotic: A staggering 41.4% of urine samples showed resistance to at least one antibiotic, signifying that nearly half of UTI cases are now challenging to treat with empiric antibiotics alone.
- Cefazolin (a 1st Gen Cephalosporin): Resistance was observed in 27.5% of cases, indicating that the once-reliable cephalosporins are becoming less effective in a substantial portion of UTI cases.
- Ciprofloxacin (fluoroquinolone): Resistance rates to ciprofloxacinwere similarly concerning, at 26.8%. Fluoroquinolones are a popular choice for UTI treatment, but resistance is on the rise.
- Potentiated sulfonamides: Resistance to sulfamethoxazole/trimethoprim (example Bactrim), another commonly used and recommended antibiotic, was observed in 16.8% of cases.
Data on file.
The implications of these resistance rates are clear: relying on cephalosporins and levofloxacin as empiric treatments for UTIs is no longer a safe bet for all patients. This necessitates a reevaluation of treatment strategies.
What Can Be Done?
In light of these findings, it's crucial to revisit UTI treatment guidelines and practices. Healthcare providers must adopt a more personalized approach to treatment and consider patient history, previous antibiotic use, and local resistance patterns. This approach can help reduce the overuse of broad-spectrum antibiotics and minimize the selective pressures on bacteria to develop resistance.
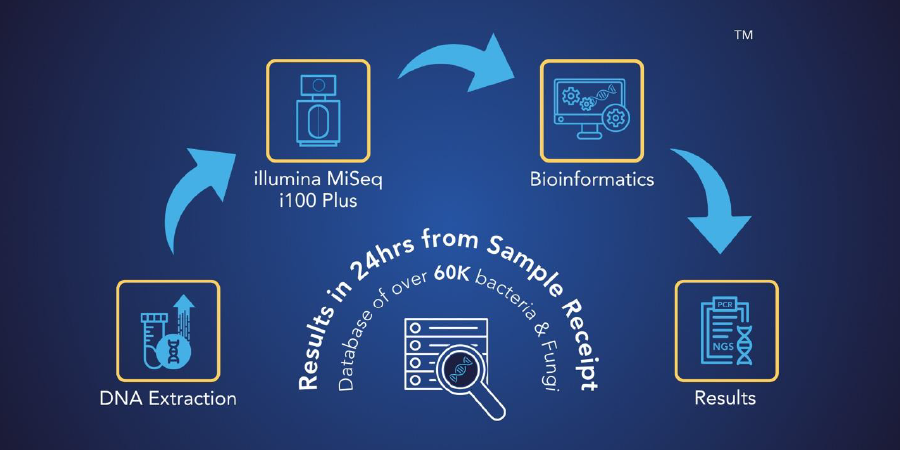
Integrating Next-Generation DNA Sequencing (NGS) technology into UTI management is a promising avenue. NGS offers a more tailored and precise approach to antibiotic treatment, as discussed in a previous blog (reference blog #1). MicroGenDX, the source of the resistance data mentioned earlier, maintains an extensive database of over 57,000 bacteria and fungi. Healthcare providers can send infectious samples to MicroGenDX for testing, enabling the identification of microbes contributing to the infection. Furthermore, their comprehensive testing for over 17 antimicrobial resistance genes offers a more detailed understanding of a patient's infection. This valuable information empowers healthcare professionals to avoid unnecessary or ineffective treatments, making NGS an invaluable tool in the fight against antibiotic resistance in UTIs.
Moreover, it's essential to promote patient education about the responsible use of antibiotics. Patients must be aware of the consequences of incomplete treatment courses, self-medication, and the importance of discussing their medical history with healthcare professionals.
Conclusion
The alarming rise in antibiotic resistance, as highlighted by the MicroGenDX study, emphasizes the need for a more thoughtful and individualized approach to treating UTIs. The days of empirically prescribing cephalosporins and levofloxacin to all UTI patients are waning. As healthcare professionals and patients work together to combat this looming threat, we can hope to preserve the effectiveness of antibiotics and ensure that UTIs are treated with the utmost care and precision. Antibiotic stewardship, responsible prescribing, better testing, and patient education are the keys to a healthier, more resilient future in the fight against UTIs and antibiotic resistance.