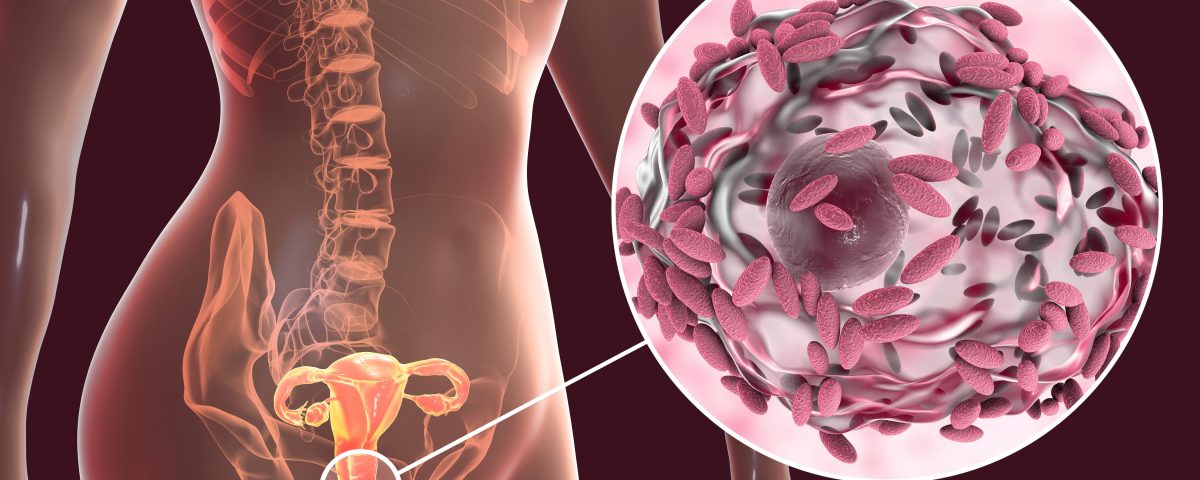
Dysbiosis of the vaginal microbiome a.k.a. bacterial vaginosis (BV) remains one of the most common vaginal infections among reproductive-aged women, affecting one in three women globally.
Despite the availability of antimicrobial treatments, recurrence rates of BV exceed 50% within three months, leading to frustration for both women and their providers. Until now, BV treatment has focused solely on women, with limited evidence backing partner treatment. However, a pioneering Australian study, Male Partner Treatment to Prevent Recurrence of Bacterial Vaginosis, published in The New England Journal of Medicine (NEJM, March 2025) provides compelling findings that treating male partners can significantly reduce BV recurrence rates.
The Link Between Male Partners and BV Recurrence
Existing epidemiological studies have long suggested that BV has characteristics of a sexually transmitted infection (STI). Men can harbor BV-associated bacteria in the penile microbiome, particularly in the urethra and subpreputial space. Prior studies failed to demonstrate a clear benefit of male-partner treatment, but many of these trials had methodological weaknesses, such as small sample sizes, inconsistent adherence tracking, and the use of single-dose oral treatments alone.
More recent randomized controlled trials (RCTs) overcome these limitations by using both oral and topical antimicrobial therapies for male partners, robustly demonstrating that BV recurrence is driven in part by bacterial exchange between sexual partners.
Study Design: Dual Therapy for Male Partners
This open-label RCT was conducted across multiple Australian health centers and enrolled 164 monogamous heterosexual couples, in which the woman had been diagnosed with BV. The study compared:
- Partner-Treatment (Experimental) Group:
- Women received standard BV treatment (oral metronidazole 400 mg, twice daily for 7 days).
- Male partners received oral metronidazole (400 mg, twice daily for 7 days) plus 2% clindamycin cream applied to the penile skin (twice daily for 7 days).
- Standard of Care (Control) Group:
- Women received the same treatment as the study group.
- Male partners received no treatment (standard care).
Key Findings: Significant Reduction in BV Recurrence
The study was halted early by the data and safety monitoring board due to the superiority of partner treatment method over the standard of care. Within the experimental treatment group:
- BV recurrence was significantly lower in the partner-treatment group (35%) compared to the control group (63%).
- Absolute risk reduction: 2.6 fewer recurrences per person-year (p<0.001).
- Longer time to recur: Women in the partner-treatment group remained BV-free for an average of 74 days vs. 54 days in the control group.
- Minimal side effects: Men reported minimal symptoms such as mild nausea (14%), headache (12%), and metallic taste (7%).
These findings provide strong clinical evidence that treating male partners interrupts the cycle of BV recurrence, addressing a key gap in existing treatment strategies.
Rethinking BV Management in Clinical Practice
A Shift Toward Partner-Inclusive BV Treatment
The implications of this study are significant for clinicians managing BV in their patients. Current BV treatment guidelines do not usually recommend male-partner treatment, but these findings suggest that an updated approach may be warranted. Considerations include:
- Reevaluating the transmission of BV: The study confirms that men can carry and transmit BV-associated bacteria, reinforcing the need for a broader treatment strategy
- Reducing Antibiotic Resistance Risk: By lowering recurrence rates, a dual therapy approach may reduce the need for repeated antibiotic courses, ultimately mitigating resistance concerns.
- Improving Patient Satisfaction and Adherence: Women who experience persistent or recurrent BV may be more likely to achieve long-term resolution with partner-inclusive treatment.
Final Thoughts: A Paradigm Shift in BV Care?
This study represents a notable breakthrough in our understanding of recurring BV and its transmission dynamics.
For healthcare providers, the evidence suggests that male-partner treatment should be factored into applicable BV management strategies, especially for patients experiencing recurring infections. It is important to note the use of a topical antibiotic for male treatment as opposed to only an oral antibiotic may have been the deciding factor in the effectiveness of male treatment.
While further research may be necessary to establish partner treatment as a universal guideline, the data strongly supports a proactive approach to reducing cases of recurring BV.
As the medical community continues to enhance and refine its approach to BV treatment, integrating partner therapy into clinical practice could provide significant benefits for patients and improve outcomes in women’s health.
If you’re interested in reading the full study, you can find it here.
For precision microbial identification in active BV cases, consider MicroGenDX’s VaginalKEY test. If you believe partner treatment is appropriate, also consider our flagship male urogenital microbiome testing product, MensKEY.